Breast Thermography is a screening that was registered with the FDA in 1982 as an adjunct to Mammography. Having a Breast Thermogram does not replace getting a Mammogram or having an Ultrasound or MRI, and like these screenings does not diagnose disease. Only a biopsy diagnoses disease.
Why Breast Thermography
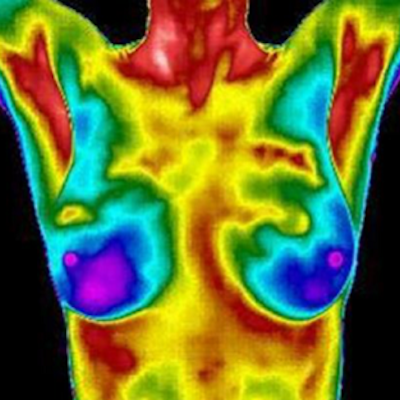
Why should women consider having a Breast Thermogram? Using a State-of-the Art Digital Infrared Camera, Breast Thermal Imaging measures heat on the surface of the breasts which may indicate inflammation (which is mapped in Rainbow Color) and irregular blood vessel patterns (which are mapped in Inverted Grayscale) that may reflect the beginning of disease or disease in progress. After the body is cooled down and then acclimated in a temperature-controlled room of 68-70 degrees, the sensitive camera measures heat differences to less than 1/10 of a degree.
A Good Analogy
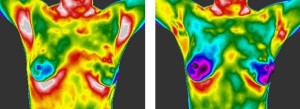
What is the best way to help people understand Breast Thermography? Using an analogy from Bruce Rind, MD, “Breast Thermography is like a Weather Forecast for Breast Health.” When the forecast is for sunny skies with no or few clouds, the risk of a storm (disease) is lower. When the forecast is for more clouds, the risk of a storm (disease) increases and when thunder and lightning is added to the forecast, the storm (disease) is here or is imminent.
Risk Assessment Scale
Following the imaging standards of the American Academy of Thermology, Bruce Rind, MD uses a Breast Thermography Risk Assessment scale of 1-5 with 1-2 being lower risk (sunny skies with no or few clouds), 3 being average risk (cloudy) and 4-5 (storm is here or coming) being above average risk. When a woman knows the State-of-her-Breast Health (i.e. her risk) and is motivated to make changes to improve her breast health, she can monitor her progress with Breast Thermography.
The goal should be and the wish is for Sunny Skies with no or few clouds for all women.